Thousands of people across Australia rallied together for the 'March for Science' on Earth Day 2017 (Saturday 22nd April) as part of a global movement to defend the vital role science plays in our health, safety, economics and government. Demonstrations were held around the world, from the North Pole to the bottom of the ocean, bringing together anyone who values the important role of science in our lives. Of late, concerns have been raised that new policies and governments are ignoring and denying scientific evidence whilst simultaneously restricting scientists' ability to research and to communicate their findings. 'Alternative facts' are being presented as viable truths in place of real scientific discoveries, and it is time for those who value science to break their silence and come forth to defend science and scientific integrity.
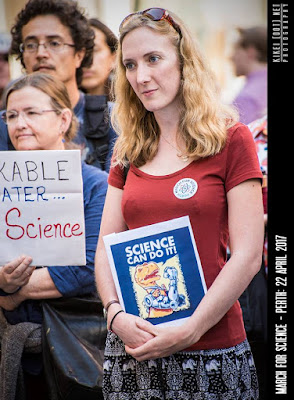 I was unsure what to expect when I headed through Forrest Place in the city centre to join the March for Science in Perth, but was overjoyed to see a large group of people adorned with science-related t-shirts, hats, banners and of course posters and signs. Having not had the opportunity to make one of my own, I was grateful to find that the organisers had a table full of extra signs for attendees and chose a dinosaur-themed sign for myself proclaiming 'Science can do it!'.
I was unsure what to expect when I headed through Forrest Place in the city centre to join the March for Science in Perth, but was overjoyed to see a large group of people adorned with science-related t-shirts, hats, banners and of course posters and signs. Having not had the opportunity to make one of my own, I was grateful to find that the organisers had a table full of extra signs for attendees and chose a dinosaur-themed sign for myself proclaiming 'Science can do it!'.
Looking around the crowd there were a variety of inventive signs and attire with slogans such as 'The Oceans are Rising and so are We!', ' There is NO Planet B' and 'Make Glaciers Great Again!'. There was even one lady with a fantastic hat decorated creatively with brightly coloured fish!
For people who are under the impression that science is of no interest or importance to them, helpful reminders such as 'Have a Smartphone? Thank a Scientist!' and 'Ever used Antibiotics? Thank Science!' demonstrated how integrated and universal science is in our lives. It was fantastic to see children and families getting involved with the March as the future we fight to secure now will be their future, and it will be their fight.
What really stood out for me was the various speakers the organisers had arranged to talk about their work and the importance of science. The main presenter (or 'MC'!) was Callum Ormonde of UWA, who is currently working on breast cancer research. Callum has gained global recognition after co-authoring a paper in 2015 on research that was awarded The Ig Nobel Prize for Chemistry for partially unboiling an egg. He has since received attention for his 2015 TEDxPerth talk and most recently was named as one of Business news WA 40 under 40 for 2017. As the main presenter, Callum was witty and engaging, effortlessly dealing with minor hiccups such as additional speakers running behind whilst entertaining the gathered crowd with ease.
Another stand out was Lindy Fitzgerald, a Professor of Neurotrauma at Curtain University who was also selected for 'Homeward Bound 2016' - an expedition to Antarctica that, as part of an international leadership and strategy program, was designed to increase the the proportion of women in higher levels of science. Taking part in this program has inspired Lindy to serve as an advocate for broader equity in science and, as a woman scientist myself, her speech was thought-provoking and empowering.
The crowd was also wowed by Professor Lyn Beazley, another neuroscientist and also WA's Chief Scientist from 2006 to 2013. In this role, Lyn acted as a science ambassador, worked closely with industry, and advised governments on science and innovation. She was also at the head of a program to supply primary schools with microscopes and has a personal goal that every Australian child with grow up to learn and love science. Inspiring future generations is essential in ensuring that the importance of scientific research and evidence continues to be upheld and it was wonderful to hear Lyn speak about something she is clearly so passionate about.
This offers just a snapshot of the amazing speakers present at the March for Science in Perth, with many more inspiring the crowd with their research, presenting evidence and explaining the importance of what they do, and how it impacts us all. Across the globe similar demonstrations were taking place, where those who love and appreciate science stood up and refused to be silenced.
For the future of human life and our planet, the application of science must influence policy and guide long-term decision making, and the March for Science demonstrated just how many people are prepared to fight for and defend science.








